Public Health Emergency Unwinding Hits Vulnerable People Hard
Lessons Learned?
Home and Community Based Service (HCBS) providers and workers poured their hearts into improving access and delivery during those three hard years. This new post PHE era is an opportunity to innovate and form new partnerships to better serve vulnerable people.
Policy makers are searching for lessons learned as our country moves forward. Unfortunately, governing bodies are using this public health emergency unwinding to go backwards to pre-pandemic operations in many states.
Medicaid HCBS Policies Changes Underway
The Kaiser Family Foundation (KFF) conducted a survey of Medicaid HCBS officials to understand what PHE policies will change this year. Keep in mind CMS offered states the right to accept a PHE extension till year 2025. Taking an extension gives state administrations the ability to incorporate new programs and approaches used during the PHE.
Reduce Services and Reimbursements
KFF reports that twenty-seven states will continue to utilize virtual eligibility assessment which enables staff to process more applicants without traveling. Twenty-one states intend to reduce client services below the PHE level. Prior Authorization restrictions will return in eighteen states which, like limiting utilization, is a cost cutting measure without disenrolling a client. Provider payment rates will be cut as well in nine states despite the ongoing labor shortage that HCBS continues to experience. KFF reports that eight states will cut home delivered meals services expanded under the PHE.
HCBS Labor Shortage Ignored
As we reported during this crisis, workforce shortages directly impacts the effectiveness of HCBS and residential care. State policy makers have short attention spans to the cries of burnout and rising mental health conditions rising in both workers and clients. Unfortunately, KFF survey reports that eleven states will cut payments to spouses, parents of minor children, and legally responsible adults from being paid. Moreover, five states are ‘firing’ family caregivers.
The Pendulum Swings Too Far
The demand for Medicaid funded services is set to explode in the coming decades. Americans are living longer and sicker than any generation in our history. I believe PHE was a fire drill for the future, yet many states are content to return to old practices rather than innovating and expanding less expensive HCBS programs to service the increasing demand.
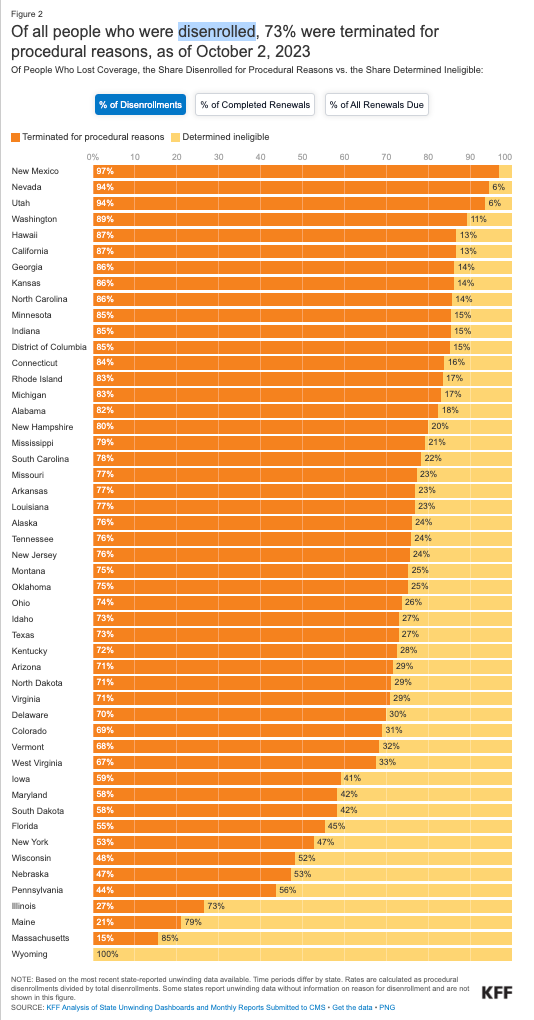
Disenrollment is a Disaster in Many States
Now, with the PHE officially over, states are restarting their processes of periodically redetermining eligibility for Medicaid. States began assessing eligibility for the 87 million Medicaid enrollees as early as February, and most states started disenrolling people by June. As of late July, almost 3.8 million people had lost their coverage. Overall, an estimated 15 million people are expected to lose Medicaid coverage during the redetermination process. Some of these individuals will qualify for no or low-cost premiums in the health insurance marketplace; others have enrolled in another health insurance plan during the pandemic.
State Government Reporting to CMS
The Centers for Medicare and Medicaid Services is requiring states to deliver monthly reports on the unwinding and disenrollment of children and adults who need the Medicaid safety net services. KFF reports 7,874,000 Medicaid enrollees have been disenrolled as of October 2, 2023, based on the most current data from 50 states and the District of Columbia. KFF warns this number is likely an undercount due to the lag in states filing their monthly report.
Oversight is Accountability, Will it Work?
Will state governments comply with these, and other, reporting requirements? How does the federal government intend to sanction state administrations without punishing the Medicaid enrollees and providers? This is a really tough nut to crack when trust within and between government actors is at such a low point. Let us use our voices to support services for vulnerable people.