Rebuilding After the Storm
The medical-industrial complex suffered a Cat 5 hurricane, EF 5 tornado and a magnitude 7.0 earthquake on the Richter scale during this pandemic. Utter devastation in every direction. Acute care became homeless, moving from the office to telehealth. Hospitals continue to assess the damage to their labor force, financing, and operations. Lastly, the long-term care sector is, well, lost in the rubble.
Health Disparities
The pandemic was not an equal-opportunity event. Studies on access to testing, treatment and vaccinations highlight the unequal care as death and case rates in minority communities outpaced whites. The Kaiser Family Foundation “ The higher rates of illness and death among people of color reflect increased risk of exposure to the virus due to living, working, and transportation situations, increased risk of experiencing serious illness if infected due to higher rates of underlying health conditions, and increased barriers to testing and treatment due to existing disparities in access to health care.”
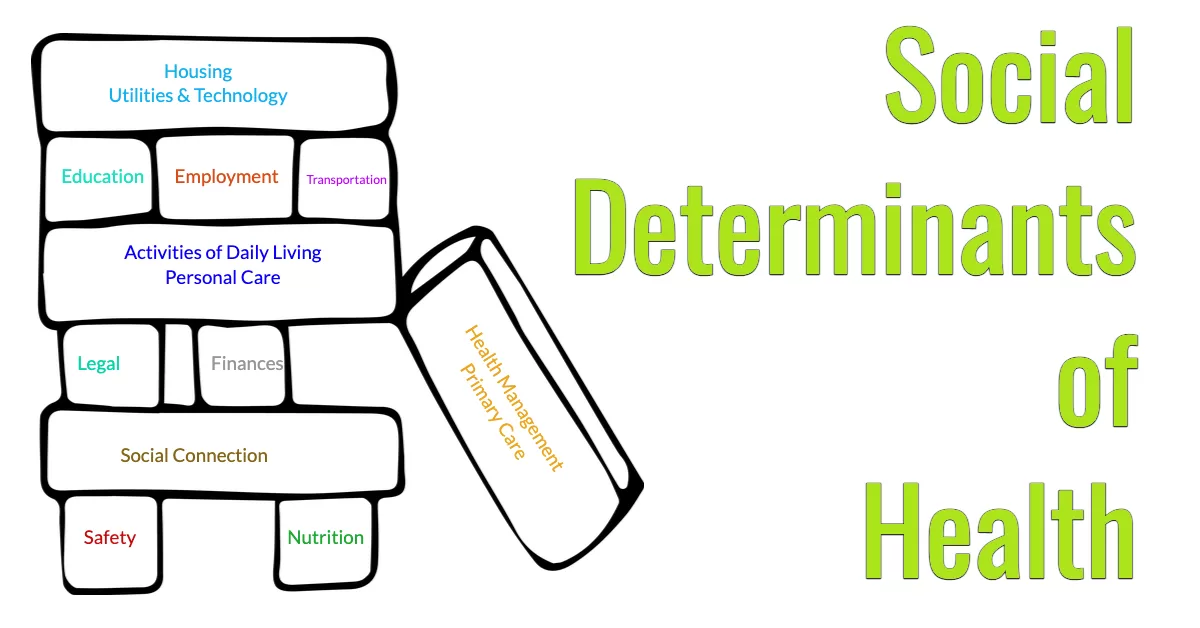
Social Determinants of Health
Think of this new model as healthcare for every day or care to reduce sick days. You see, social determinants of health (SDOH) encompass the way we live, learn, work and play. Imagine the impact our care dollars can achieve when we collect, protect and properly share this information on food, housing, transportation, community safety and all the other “non-clinical” factors of living during a care episode. Then, we share this data with community-based organizations and other service providers to address the SDOH that persist beyond a healthcare episode. A few examples of SDOH impact.
- The risk of serious illness after being infected with the Coronavirus are higher among people with low-income households
- 80% of sickness is attributed to social factors
- Loneliness and social isolation are as deadly as smoking 15 cigarettes.
- Many chronic illnesses and mental health problems are made worse by exposure to violence.
- Homelessness and housing insecurity amplify anxiety, fear, depression, and sleeplessness. In fact, increased rates of mental illness and substance use are common.

Turning Disaster into Opportunity
Do you remember the story of Greensburg, Kansas? In 2007, this community of 1,383 people experienced a EF5 tornado that wiped out 95% of the town. I encourage you to watch this short video and listen to the resilience in the Greensburg residents.
Reimagining Care
Apply this same sentiment to our nation’s healthcare system. The Office of National Coordinator (ONC) in the US Department of Health and Human Services, is rebuilding our care system to address the Social Determinants of Health at the macro, mezzo, and micro-levels of care, like these examples of new care delivery models:
- Special Needs Population programs for communities, institutions and dual enrolled (Medicare and Medicaid) individuals with person-centered care.
- Medicare Advantage plans with funding for home modification, nutrition, home care and other home-based services
- Expansion of telehealth and remote patient monitoring services increase the opportunities for healthcare delivery in the home.
- Funding to build a more robust and responsive public health system increases our community and national readiness for the next pandemic.
Early signs indicate our new care system should be smarter, more agile, and person-centered in response to health disparities exacerbated by the pandemic. Stay tuned to learn more about how you and your organization can address the Social Determinants of Health movement.