The medical-industrial complex suffered a Cat 5 hurricane, EF 5 tornado and a magnitude 7.0 earthquake on the Richter scale during this pandemic. Utter devastation in every direction. Acute care moved from the office to telehealth. Hospitals continue to assess the damage to their labor force, financing, and operations. Lastly, the long-term care sector, well, the search for survivors continues on.
Health Disparities
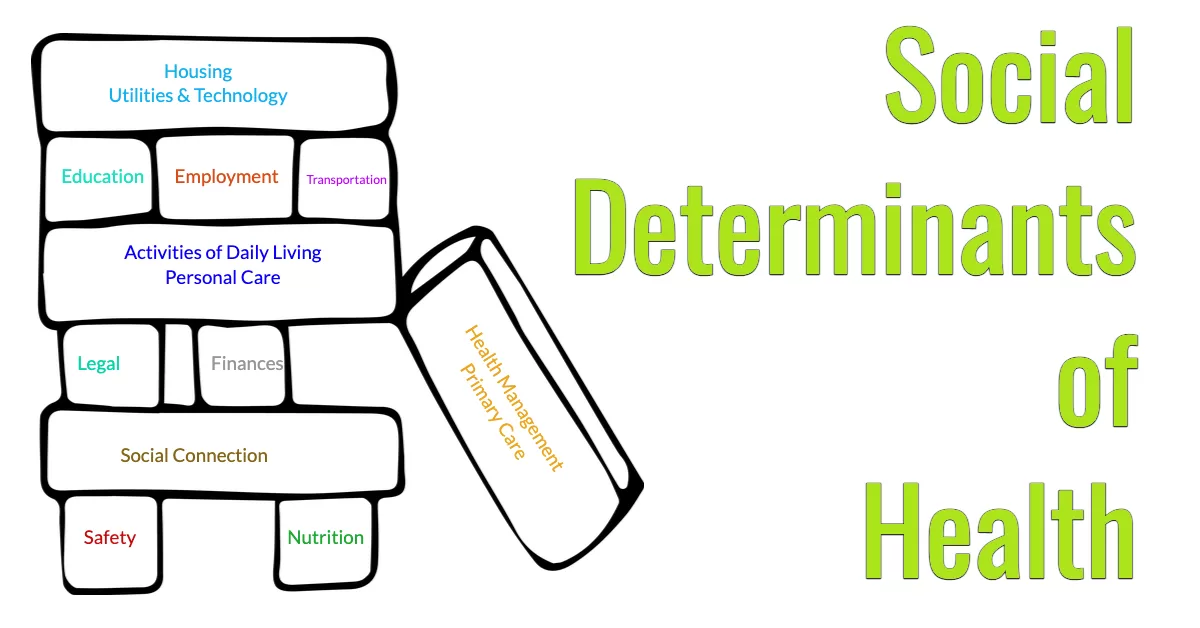
The pandemic was not an equal-opportunity event. Studies on access to testing, treatment and vaccinations highlight unequal care as death and case rates in minority communities outpaced whites. The Kaiser Family Foundation paper on health disparities points out “The higher rates of illness and death among people of color reflect increased risk of exposure to the virus due to living, working, and transportation situations, increased risk of experiencing serious illness if infected due to higher rates of underlying health conditions, and increased barriers to testing and treatment due to existing disparities in access to health care.”