Caregivers Expanded Role and Access to the Healthcare Team
Caregivers Expanded Role and Access to the Healthcare Team
Patience Comes to Those Who Wait
As a medical social worker, I can attest that the changes announced for the 2025 Medicare fee schedule are long overdue. According to the recent announcements, the Centers for Medicare and Medicaid Services (CMS) will now pay for caregiver training and support before and after discharge from an acute care hospital stay. These changes require physician practices to change which may or may not happen due a cut in their reimbursements.
The announced 2025 fee schedule changes on the Current Procedural Terminology (CPT) codes published by CMS finally gives caregivers a seat on the healthcare team. These updates reflect a growing recognition of the critical role caregivers play in the healthcare continuum, particularly in managing chronic illnesses and providing essential care to vulnerable persons at home. CMS recognizes caregivers as “an adult family member or other individual who has a significant relationship with, and who provides a broad range of assistance to, an individual with a chronic or other health condition, disability, or functional limitation,” or “a family member, friend, or neighbor who provides unpaid assistance to a person with a chronic illness or disabling condition.”
The big news here is status of the family caregiver in the eyes of CMS. Caregiver training is no longer contingent on the patient being present. CMS now considers that “training in strategies and techniques to facilitate the vulnerable person’s functional performance in the home or community as reasonable and necessary” for treatment after the plan of care is established. This is a significant change that acknowledges some patients may not be capable to carry out care plan tasks independently, think of medication or IV therapy management. If properly enacted, this change should reduce hospital readmissions, provide support for the caregiver, and improve the care plan goals and strategies to meet the patient’s abilities and resources.
Telemedicine Expansion for Caregiver Training Services
The pandemic accelerated the growth of telehealth services. However, the Caregiver Training Services (CTS) codes in the CPT codes, if used properly, expands who and how education and support for caregivers. The shift to include telemedicine list is a monumental step forward, acknowledging the necessity for caregivers to receive training in real-time and within the comfort of their homes. This level of on-demand support is a game changer.
CTS telehealth enables training without the need to travel, which can be particularly beneficial for those in rural areas or those managing complex schedules. The ability to receive training virtually means that caregivers can more readily apply new skills and techniques immediately, thereby improving a person’s outcomes.
The announcement explicitly states that CMS will monitor the efficacy of these telemedicine services over the year to determine if they should be permanently added to the list. Keep in mind, this provisional period is crucial for assessing the impact and ensuring that telemedicine can effectively deliver the needed training. I will be watching to see how this monitoring is structured.
New Codes for Direct Care Tasks
I have spoken to family caregivers managing a picc line or giving injections based on quick hospital bedside instruction by a very busy nurse, they are not adequately trained. Family caregivers perform nursing tasks without the benefit of a college education. To bridge this vast training gap, CMS has also introduced new codes for CTS that cover ‘direct care’ tasks, such as wound care, infection control, and medication administration. These tasks are often critical for care plan success and require precise and skilled execution to prevent complications and ensure vulnerable person safety.
By recognizing these tasks within the fee schedule, CMS highlights the importance of equipping caregivers with the necessary skills to perform hands-on treatments that were traditionally managed by nursing professionals. This not only empowers caregivers but also helps bridge the gap in healthcare delivery, particularly in home settings where professional medical assistance may not be immediately available. Training in these areas can significantly reduce the risk of complications, hospital readmissions, and improve overall patient health outcomes. For instance, proper wound care techniques can prevent infections, while effective medication administration can ensure that vulnerable persons adhere to their treatment plans accurately.
Personalized Behavioral Management Training
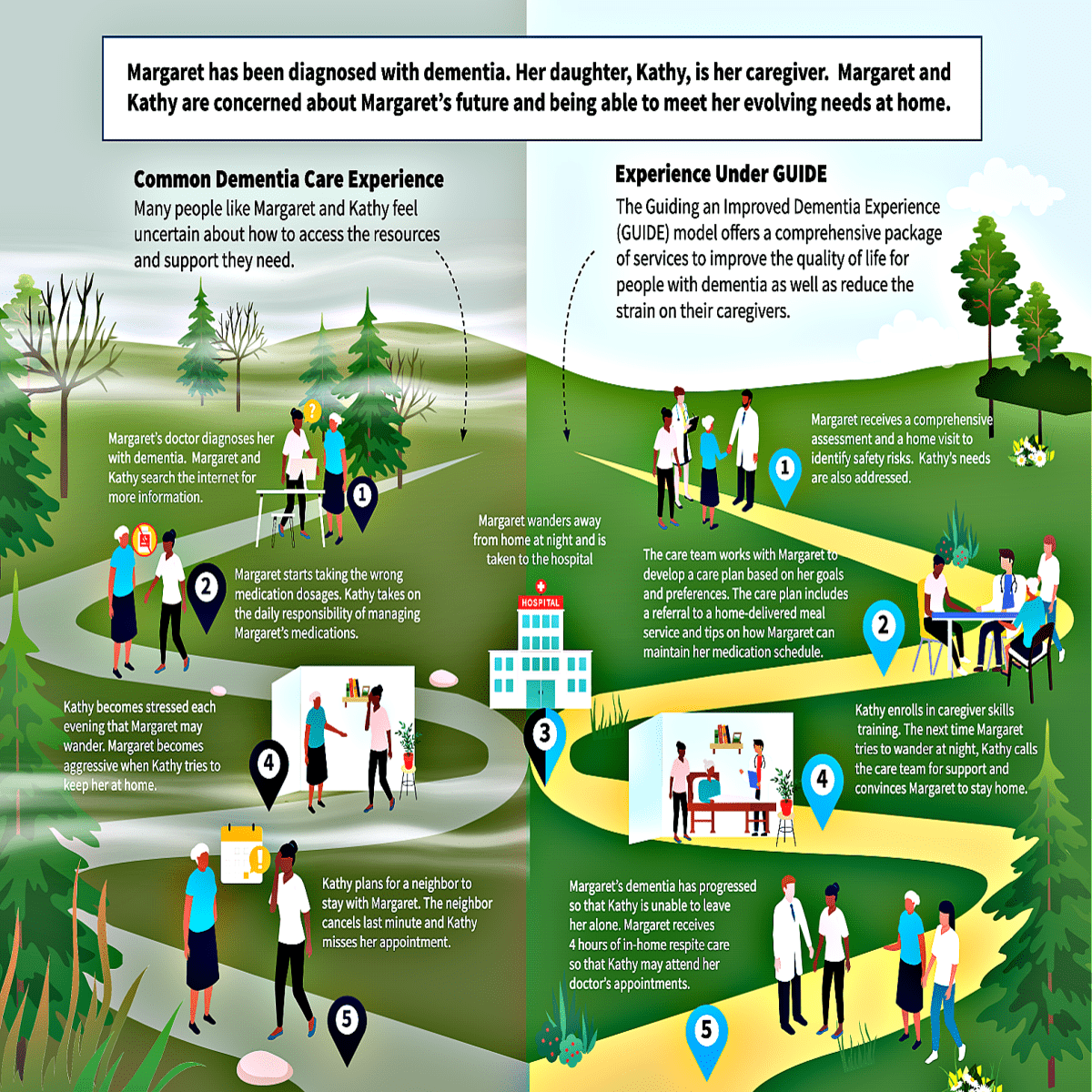
In addition to direct care tasks, CMS has expanded its support for caregiver training in behavioral management and modification. While 2024 codes focused on group-based training, the new 2025 codes recognize the need for one-on-one training sessions. This is particularly relevant for caregivers managing persons with mental health issues such as depression, substance use disorders, dementia disorders, or challenging behaviors.
If enacted as conceived, this training provides a tailored approach, allowing caregivers to address specific challenges unique to their situation. Personalized training can significantly enhance the caregiver’s ability to manage difficult behaviors effectively, leading to better vulnerable person outcomes and reducing caregiver stress.
Behavioral management training is essential for caregivers dealing with vulnerable persons who may exhibit aggressive, non-compliant, or otherwise difficult behaviors. With the right training, caregivers can implement strategies to modify these behaviors, fostering a safer and more supportive environment for both the person and the caregiver. The GUIDE model in the illustration below is an example of the progress CMS is making in this area.
Assessing Caregiver Training Needs
The age friendly hospital movement deserves accolades for advancing caregiver training and education needs. Another noteworthy update is the allowance for existing CPT code 96161 to be used to assess a caregiver’s training needs. This code can now be utilized to evaluate a caregiver’s current skills, knowledge, health risks, and other considerations that may influence the type and extent of training required. Tracking how and when CPT code 96161 is used in 2025 could give us a window into the impact of these changes to CTS.
Credit for Caring was conceived, designed, and remains committed to supporting care teams in properly assessing a person’s needs and resources. This assessment is a crucial step in providing tailored training programs that meet the specific needs of caregivers. By identifying gaps in knowledge and skills, healthcare providers can develop more effective training plans that enhance the caregiver’s ability to provide quality care. In fact, we offer free daily activities, home safety and community resource check-ups for all.
Verbal Consent Removes Barriers
In 2024, CMS required written consent to be documented in the medical record before conducting caregiver assessments or training. This year, CMS has eased this requirement by allowing verbal consent, which simplifies the documentation process and reduces administrative burden. In fact, verbal consent can streamline the initiation of caregiver training services, making it more accessible and less cumbersome for both caregivers and healthcare providers. This change reflects a more practical approach to consent, ensuring that necessary training can commence promptly without unnecessary delays.
Applauding Progress
Let’s celebrate a win today. These changes not only empower caregivers with the skills and knowledge needed to provide high-quality care but also recognize the importance of flexibility and accessibility in training delivery. The inclusion of telemedicine options and simplified consent procedures are particularly beneficial, making it easier for caregivers to access the resources they need without added stress. In addition, healthcare providers can leverage these updates to offer more comprehensive support to caregivers, ultimately leading to better patient outcomes and a more efficient healthcare system. The ability to assess caregiver needs and provide targeted training can enhance the overall quality of care, reduce hospital readmissions, and improve satisfaction. I will update you on the implementation of these essential changes next year.
Share This Story, Choose Your Platform!
About the author : Monica Stynchula
Credit for Caring: Your Modern DIY Aging in Place Feeling overwhelmed? We've got you! Expert tips, safety products, & innovative solutions for solo agers, families, and communities. Personalized plans, must-have resources, & a supportive community await. Save big & simplify caregiving: Creditforcaring.com